Osteochondrosis is a pathology in which the intervertebral discs that separate the vertebrae are destroyed. Degenerative-dystrophic changes in tissues can develop at different rates and manifest with different symptoms. The clinical picture depends on which part is affected and what caused the disease.
general characteristics
Destructive processes in the spine can lead to irreversible consequences that significantly complicate a person's life. They can affect any of the regions (cervical, thoracic or lumbar) or extend to the entire spine.
In most cases, osteochondrosis occurs in waves: periods of exacerbations alternate with periods of remission. In this case, 3 flow options are possible, of different nature:
- progressive - each subsequent exacerbation is accompanied by more severe symptoms, the intervals between them are reduced;
- receding - the frequency and intensity of attacks constantly decreases;
- stable - exacerbations occur regularly with the same symptoms.
It is also worth noting that damage to different parts of the spine not only manifests itself differently. The therapeutic approach and treatment methods also have their own characteristics.
Stages
Pathological changes in discs and vertebrae do not appear immediately. Its development is preceded by a deterioration in blood circulation and nutrition of paravertebral (paravertebral) structures, caused by external and internal factors.
Degeneration of osteochondral tissue occurs in all people with age and is one of the signs of aging of the body. However, this process can be dramatically accelerated after an injury or as a result of general illness.
The early appearance of chondrosis is greatly facilitated by overload of the back, both dynamic and static, when a person is forced to stay in the same position for a long time.
Cervical osteochondrosis occurs in 3 stages, each of which is characterized by its own manifestations:
- Level 1. Headaches and discomfort in the neck and back of the neck occur periodically;
- Stage 2. Headaches become more frequent, you sometimes feel dizzy, and performance decreases. It is at stage 2 that patients most often consult a doctor, but it is no longer possible to achieve complete restoration of damaged structures;
- Stage 3, final. It is characterized by large-scale damage to the vertebrae, discs and ligamentous system. It manifests itself as severe and almost constant headaches, loss of coordination of movements, stiffness in the cervical spine, as well as decreased vision and hearing.
Some experts distinguish 4 stages of osteochondrosis: the last is accompanied by an almost total loss of mobility and severe neurological symptoms.
From one stage to another, the nucleus pulposus of the disc loses moisture, and with it elasticity disappears and shock absorption qualities decrease. The intervertebral disc dries out, flattens and cracks. Neighboring vertebrae move closer together, which, in turn, causes displacement of the facet joints. All of this causes pinching of the spinal nerves, pain and other symptoms.
IMPORTANT: therapy for osteochondrosis of stages 2 and 3 is reduced to preventing relapses and maximizing the remission phase.
Causes of exacerbation
For cervical chondrosis to worsen, exposure to one or more factors is necessary, among which doctors call:
- increased loads on the back and spine associated with lifting heavy weights or changing the training program of athletes;
- psychoemotional overload;
- massage or manual therapy procedures performed by an unqualified specialist;
- seasonality: in spring and autumn, exacerbations occur more frequently;
- hormonal imbalances during pregnancy and menopause;
- the presence of chronic diseases that weaken the body, including frequent colds;
- sudden weight gain.
Symptoms
An attack of cervical osteochondrosis can begin with the appearance of discomfort in the shoulder girdle and occipital region. At the same time, general well-being deteriorates, the person gets tired quickly and copes worse with professional and everyday responsibilities.
Sometimes a sudden exacerbation occurs with severe headaches. Often (in 72% of cases), certain signs indicate the proximity of an attack, in particular, a feeling of heaviness in the head, dull pain in the neck and shoulder girdle. Symptoms usually worsen in the morning.
The symptoms of exacerbation of cervical osteochondrosis have significant similarities with the general clinical picture of this disease. The main symptom is pain of different intensity and nature. The neck and head may hurt on one or both sides. Often the pain extends to the collarbone area and shoulders. For some people, painful sensations occur only when turning or tilting the head or moving the arm.
IMPORTANT: Sometimes cervical chondrosis "masks" as a heart attack and causes pain behind the sternum, under the scapula and in the left arm.
Signs of acute osteochondrosis may also include:
- dizziness;
- worsening sleep, decreased concentration, memory problems;
- flickering spots before the eyes, noise and ringing in the ears;
- nausea that turns into vomiting;
- violation of diction;
- Sensitivity disorder in the neck and arm.

There are no "painless" variants of the course of osteochondrosis; damage to any of the sections is manifested by pain of different localization and intensity;
Cervical chondrosis cannot be ignored; Without treatment, it will not only worsen more frequently, but can also cause a serious complication in the form of a stroke. The cause of acute stroke is compression of the large arteries that supply the brain.
How long does an exacerbation of cervical osteochondrosis last?
The duration of the attack depends on the factor that provoked it, the season of the year and the general state of health of the person, as well as the treatment methods. The exacerbation is more difficult to tolerate and lasts longer in the cold season.
On average, the acute period lasts from 4 days to a week, then the pain gradually subsides, which takes about three more weeks. The total duration of the exacerbation is one and a half months.
To do
The best thing you can do if you suspect cervical chondrosis is to visit a neurologist or orthopedist. He will prescribe the necessary studies, find out what leads to exacerbations and prescribe appropriate treatment.
Before visiting the doctor, it is advisable to avoid any tension in your back and adopt the most comfortable position. It is recommended to lie on a flat, elastic surface to relax the neck muscles as much as possible and reduce the intensity of the pain. It is advisable to isolate the painful area with a scarf, handkerchief or wrap yourself in a blanket.
It is very important to immobilize the cervical spine and try not to turn or tilt your head too much. For this, doctors even recommend using special orthopedic collars. You can make them yourself with cotton and cardboard or buy them at the pharmacy.
IMPORTANT: the orthopedic collar is not worn more than four hours a day; Otherwise, it will cause harm instead of benefit and recovery will be delayed.
The most famous of the collars is the Shants collar. This is an indispensable tool for temporary unloading and stretching of the spine in the cervical region. Despite its rather rough appearance, such a splint, when correctly selected, provides comfort and significantly reduces pain.
Severe pain is relieved with analgesics. The most effective drugs belong to the group of NSAIDs, non-steroidal anti-inflammatory drugs.
If osteochondrosis worsens, it is prohibited to heat the sore spot in any way: with hot ointment, applying mustard plasters or compresses, or taking a steam bath in a sauna. Do not massage the affected area or self-medicate.
Treatment
Treatment of exacerbation of cervical osteochondrosis is carried out by medicinal and non-medicinal methods. The latter include physiotherapy, massage and gymnastics. Traditional medicine can have a good effect, as long as it is in agreement with the treating doctor.

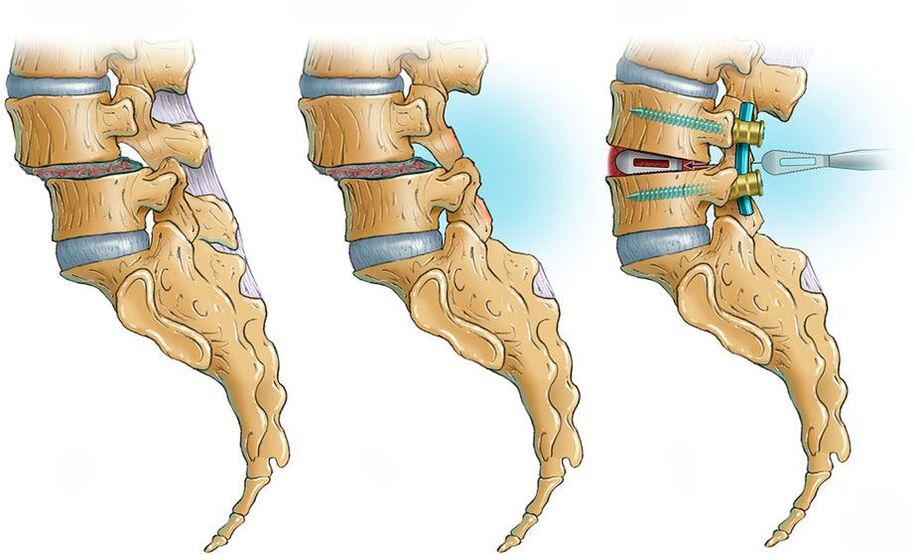
Surgical treatment of osteochondrosis is carried out only in extreme cases and consists of partial or complete removal of hernias, osteophytes (bone growths)
In the acute period, the main efforts are aimed at relieving pain. Depending on their intensity, pain relievers and NSAIDs are prescribed in the form of injections or tablets. These can be drugs based on substances diclofenac, ibuprofen, nimesulide, metamizole sodium. In addition to them, it is recommended to use anti-inflammatory ointments.
Muscle relaxants will help relieve muscle spasms. If there is swelling, diuretics are prescribed, which remove excess fluid and thus reduce pressure on the nerve endings.
Once the acute symptoms have been eliminated, vitamin complexes containing vitamin B are added to the treatment; nootropics that normalize the transmission of impulses along nerve fibers; chondroprotectors for the restoration and strengthening of the cartilaginous tissue of the intervertebral discs.
Physiotherapy
Physiotherapy, which can be prescribed in the subacute phase and continued during the period of remission, helps to quickly relieve the exacerbation of cervical osteochondrosis. They help improve blood supply to the damaged segment, relax muscles and reduce pain and inflammation. Traditionally, electrophoresis, ultrasound, magnetic resonance imaging, and cryotherapy (cold treatment) are considered the most effective methods.
At the beginning of the remission period, massage sessions are prescribed, which can be carried out both in a specialized office and at home on your own. It is best to practice both.
exercise therapy
If chondrosis of the cervical spine has worsened and is accompanied by severe pain, the person is prescribed strict bed rest. As the pain decreases, they first move to semi-bed rest and then to a gentle motor regime.
It is useful for all patients with any stage of chondrosis to sleep on an orthopedic mattress and pillow. These accessories maintain the anatomically correct position of the body and relieve stiffness and pain in the morning thanks to gentle traction on the spine. In hospitals, a Glisson loop is used for this.

The preferred positions for cervical chondrosis are on the side and on the back. An important condition is a comfortable and "correct" pillow, preferably orthopedic.
When the acute pain passes, physiotherapy exercises are started. In combination with other methods, its effectiveness is very high. The first training sessions should be carried out under the supervision of an instructor who will select and teach how to perform the exercises correctly.
IMPORTANT: the tempo and amplitude must be increased gradually, expanding the program over time and increasing the load.
Gymnastics according to Bonina
- While sitting or standing, raise your arms. With an inhalation, connect your fingers at the top and lower your clasped hands. The collar stays in place.
- Half rotation of the shoulders. Pull your shoulders back, drawing an arc in the air and return it following the same arc.
- Stretch your head forward and stay in this position for a few seconds.
- Turn your head now to the right, now to the left, each time looking over your shoulder.
- At the same time, raise your right shoulder and lower your left shoulder.
Gymnastics according to Bubnovsky
- Sitting in a chair, turn your head to the right and lower your chin to your shoulder, stay in this position. Then repeat the exercise on the left side.
- Tilt your head toward your chest, while slightly pulling your neck forward and up.
- Turn your head with your chin up, first to the right and then to the left. Then repeat the exercise by raising your hands and joining your fingers.
- Place your left hand on your right shoulder and turn your head to the left. Hold the position for a few seconds and turn your head to the right, placing your right hand on your left shoulder.
- Place your hands on your hips and slowly stretch, moving your back back and lifting your neck.
- Starting position: standing, head down. Gently move your chin first to the right and then to the left shoulder, each time lowering it to the midpoint of the chest.
Traditional methods
Treatment of cervical osteochondrosis at home includes water and warming procedures, and the use of orthopedic devices. Lotions and compresses made from vegetables and herbs are always in demand and popularity.
In case of exacerbation, you can take a warm shower and wrap your neck with a warm scarf. To reduce pain and inflammation, lotions are made from herbs, for example, sage and mint. To prepare a healing solution, brew one or two tablespoons of the herb in a glass of boiling water and leave for 15 to 20 minutes. After cooling to a comfortable temperature, soak a cotton ball or bandage and apply it to the painful place for 10 to 20 minutes. The procedure is performed up to 4 times a day.
The onion compress is prepared with grated or chopped onion in a blender. The resulting mass is distributed on gauze and applied to the neck, covering the top with plastic wrap and a cotton cloth. After 2-3 hours, the compress is removed and the skin is washed with warm water.

Therapeutic compresses are a simple, affordable and very effective treatment method if used correctly.
Application with kerosene is done like this: a linen or cotton cloth (you can use gauze or a bandage) is dipped in kerosene and applied to the neck area. Cover the top of the pad with cotton or polyethylene to prevent it from spreading. Leave it on for no more than three hours; If a strong burning sensation occurs, remove immediately and rinse with water.
As an ambulance for acute chondrosis of the cervical vertebra, a product with the following composition is used:
- 5 Analgin tablets crushed into powder;
- ethyl alcohol – 15 ml;
- camphor alcohol – 5 ml;
- iodine – 5 ml.
Mix everything and rub on the skin over the painful area.
Osteochondrosis can also be treated "from within", taking, for example, an infusion of pine buds. In this recipe, pharmacy lists or fresh ones, collected in early spring, are used. Fresh buds must be cut beforehand.

For medicinal purposes, it is better to use medium-sized buds, as they contain more useful substances.
Raw materials are covered with sugar in a 1: 2 ratio and infused for two weeks. Use the finished product one teaspoon three times a day. To enhance the effect, it is necessary to keep it in your mouth for a while and only then swallow it. The course of treatment is up to three weeks.
Things to consider
All doctors insist that the early stages of osteochondrosis go almost unnoticed and are not particularly disturbing. At this stage, when the symptoms are limited to slight discomfort and slight stiffness in the morning, it can only be cured with the help of exercise therapy. You won't need medication, but you will have to adjust your diet and lifestyle.
The best prevention of both the disease and its relapses is physical activity. Regular physical exercise will maintain good posture and help prevent the development of destructive processes in the spine.
In severe and advanced cases a lot can also be done. The systematic implementation of therapeutic gymnastics complexes and drug treatment will significantly improve well-being and reduce the risk of new exacerbations.
Frequently asked questions
What symptoms of exacerbation of cervical osteochondrosis can occur?
During an exacerbation of cervical osteochondrosis, the patient may experience pain in the neck, shoulders, arms, dizziness, a feeling of numbness or tingling in the arms, as well as limited mobility of the neck.
What factors can provoke an exacerbation of cervical osteochondrosis?
Exacerbation of cervical osteochondrosis can be caused by overload of the neck, prolonged stay in an incorrect position, trauma, stress and age-related changes in the spine.
What methods of treatment for exacerbation of cervical osteochondrosis can be effective?
To relieve the symptoms of exacerbation of cervical osteochondrosis, non-drug methods (massage, physiotherapy, exercise), drug therapy and, in some cases, surgical intervention can be used.
Helpful tips
Tip #1
Maintain correct posture and avoid remaining in an incorrect position for long periods of time. Do neck and back exercises regularly to strengthen muscles and improve flexibility.
Tip #2
Avoid sitting in front of a computer or monitor for long periods of time. Take regular breaks to stretch your neck and back, do eye exercises, and neck and shoulder relaxation exercises.
Tip #3
Use a pillow and mattress that supports the correct position of your neck and back while you sleep. This will help reduce the load on the spine and prevent exacerbation of osteochondrosis.



































